
Systems thinking is an approach that views healthcare not as a collection of isolated tasks or departments, but as a complex, adaptive system made up of interrelated functions, people (e.g., healthcare workers, patients, families) and environments.
It recognizes that outcomes, both positive and negative, emerge from interactions and variability across the system. To improve care, we must understand how it is actually delivered and experienced in practice, not just how it is intended or imagined.
The Functional Resonance Analysis Method (FRAM) is a systems-thinking tool designed to model the complexity of real-world work, especially in healthcare settings.
FRAM reveals the often-invisible interactions and variabilities that shape system performance, particularly the gap between Work as Imagined (WAI)—how work is expected to occur at the organizational or policy level—and Work as Done (WAD)—how work actually unfolds at the clinical level.
The closer one is to direct care, the more accurate the understanding of how healthcare functions in practice.
The Functional Resonance Analysis Method (FRAM) uses a structured, stepwise approach to model and analyze complex healthcare processes:
Clearly identify the goal of the analysis and specify the process or system to be examined.
Determine the key activities (functions) that make up the process. These can be human, organizational, or technological, and are interdependent by nature.
Data is gathered through interviews, focus groups, observations and document review.
Each function is described using six aspects:
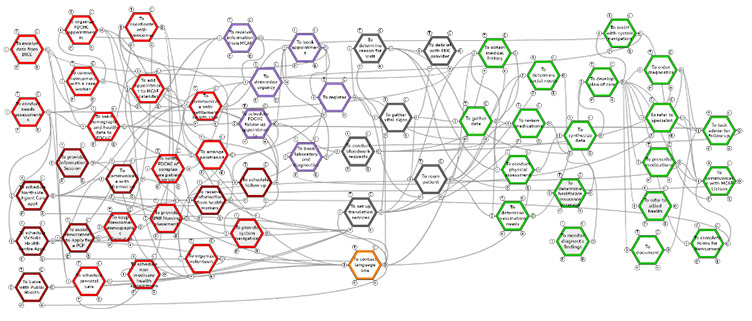
Functions are then mapped visually (e.g., using the FRAM Model Visualizer) to show how they are “coupled,” or interconnected through shared aspects.
Examine how functions influence each other and how variability in one may affect others, revealing system dynamics.
Assess how early (upstream) variability can ripple through the system and affect later (downstream) outcomes.
Identify how to dampen negative variability, enhance resilience, and develop interventions that align with how work is actually done.
The FRAM is a research approach that helps our lab bridge the gap between idealized workflows and the lived reality of healthcare delivery.
It captures the complexity of direct service work and enables a nuanced understanding of both the intended and actual delivery of care.
Through this approach, we can work with health and social care sectors, clinicians, and community organizations to identify system strengths and vulnerabilities, understand performance variability and develop improvements that are grounded in how work truly happens.